The newest COVID-19 variant is so contagious that even people who’ve avoided it so far are getting infected and the 80% of Americans who’ve already been infected are likely to catch it again, experts say.
Essentially, everyone in the country is at risk for infection now, even if they’re super careful, up to date on vaccines or have caught it before, said Paula Cannon, a virologist at the University of Southern California.
“It’s crazy infectious,” said Cannon, who is recovering from her first case of COVID-19, caught when she was vacationing over the holidays in her native Britain.
“All the things that have protected you for the past couple of years, I don’t think are going to protect you against this new crop of variants,” she said.
The number of severe infections and deaths remains relatively low, despite the high level of infections, she said, thanks to vaccinations – and probably – previous infections.
The latest variant, called XBB.1.5, grew exponentially over the month of December, from about 1% of cases nationwide to 40% as of Dec. 31, according to data from the Centers for Disease Control and Prevention. The variant is likely behind the vast majority of cases in New York and New England.
Its growth is probably due to XBB.1.5’s characteristics – it appears to bind even more tightly to receptors in the human body than its predecessors – as well as human behavior, such as traveling and not masking.
It’s a good idea to do what you can to avoid getting infected, said Dr. Ziyad Al-Aly, chief of research and development at the VA St. Louis Health Care System and a clinical epidemiologist at Washington University in St. Louis.
It’s still early and there are a lot of unknowns about XBB.1.5, he said. Every infection makes someone vulnerable to a bad course of the disease and to the lingering, miserable symptoms of long COVID, Al-Aly’s research shows.
“Reinfection buys you additional risk,” he said.
As the United States enters the fourth year of COVID-19, we’re providing an update on the state of the pandemic. Here’s a preview of what you’ll learn in this article:
What to know about XBB.1.5 symptoms and how long they last
COVID-19 symptoms typically last around five to seven days and can include fever, sore throat, muscle aches, exhaustion, nausea, cough and sinus congestion, among other problems.
Symptoms with XBB.1.5 are the same as with earlier variants and can range from almost nothing to shortness of breath and low oxygen levels that require emergency medical attention.
Early in the pandemic, COVID-19 often cost people their sense of taste and smell, at least temporarily, but that symptom seems less common, possibly because of vaccination or previous infection rather than a change in the virus, said Dr. Peter Hotez, an infectious disease specialist and co-director of the Center for Vaccine Development at Texas Children’s Hospital.
How long does COVID last? How long are you contagious?
It takes anywhere from two to 14 days for exposure to lead to symptoms and a positive test.
People with COVID-19 are contagious as long as they remain positive on a rapid test, typically for about 10 days, but often longer.
The CDC recommends people isolate for at least five days and wear an N95 or similarly protective mask for at least 10 days when around others. Day One is considered the first full day after symptoms start.
A PCR test, which is considered the gold standard for diagnosing COVID-19, can remain positive for months because it detects viral fragments as well as the whole, infectious virus. To confirm the end of the contagious period, experts instead recommend a negative rapid test after 10 days or two within 48 hours if sooner.
Can you get COVID more than once?
Yes. While a previous infection provides some protection, that fades over time and as the virus evolves into different variants.
Some people who had a mild case with a first infection get hit harder the second or third time, while others might suffer less.
“Even if you’ve had it before, that doesn’t mean your next bout is going to be the same,” Cannon said. There are lots of factors at play in determining the seriousness of an infection, she said, including prior immunity, the nature of the variant and how long it’s been since your last infection or vaccination.
It’s possible that her recent infection was much milder than her husband’s, for instance, because she had caught a head cold a few days earlier, while her husband hadn’t. A respiratory virus can put the immune system on high alert and might have provided some protection when she was exposed to COVID-19.
“It’s part of the bigger dance between our bodies and our immune system,” Cannon said.
How to avoid infection
The methods for avoiding infection haven’t changed, though it can be hard to stick with them when no one else is: Get vaccinated, wear a mask and avoid crowded spaces.
First is getting vaccinated. This will protect against severe infection as well as reduce the risk of passing the virus to others, said Hotez, also dean of the National School of Tropical Medicine at Baylor College of Medicine.
The newer boosters, which take aim at both the original virus and the BA.4/BA.5 variants common this summer, are more protective against XBB.1.5 than earlier boosters. People who are up to date on their COVID-19 shots probably don’t shed as much virus for as long, so they’re also less likely to pass it on, he added.
Past infection provides some protection against severe disease, but that protection is “highly unreliable,” Hotez said.
Second is wearing a mask. Good quality, well-fitting masks, like an N95 or KN95 can reduce the risk of infection.

Cannon said people sometimes get annoyed at her mask-wearing “because it’s like I’m reminding them that (COVID) is still a problem.” But she doesn’t want to accidentally pass COVID on to someone who might be more vulnerable to the virus.
Third is avoiding crowded indoor spaces. You’re less likely to get infected in large indoor spaces with high ceilings and lots of ventilation than in cramped, airless ones.
What to do if you get sick
It’s a good idea to have a plan ready in case you get sick, Cannon said. She suggests every plan include:
- How to isolate from others in your household
- The contact number for a health care provider who can prescribe an antiviral
- Equipment such as rapid coronavirus tests, extra masks, a thermometer and a pulse oximeter to make sure the patient’s blood oxygen level doesn’t drop below the low 90s
Every U.S. household is eligible for four free coronavirus tests from the government that can be ordered from this link: covid.gov/tests.
For someone over 60 or with medical conditions like obesity that raise the risk for serious disease, the first step after a positive test should be a call to the doctor to get the antiviral Paxlovid, she and others said. The government has pre-bought millions of doses, so they are available for free.
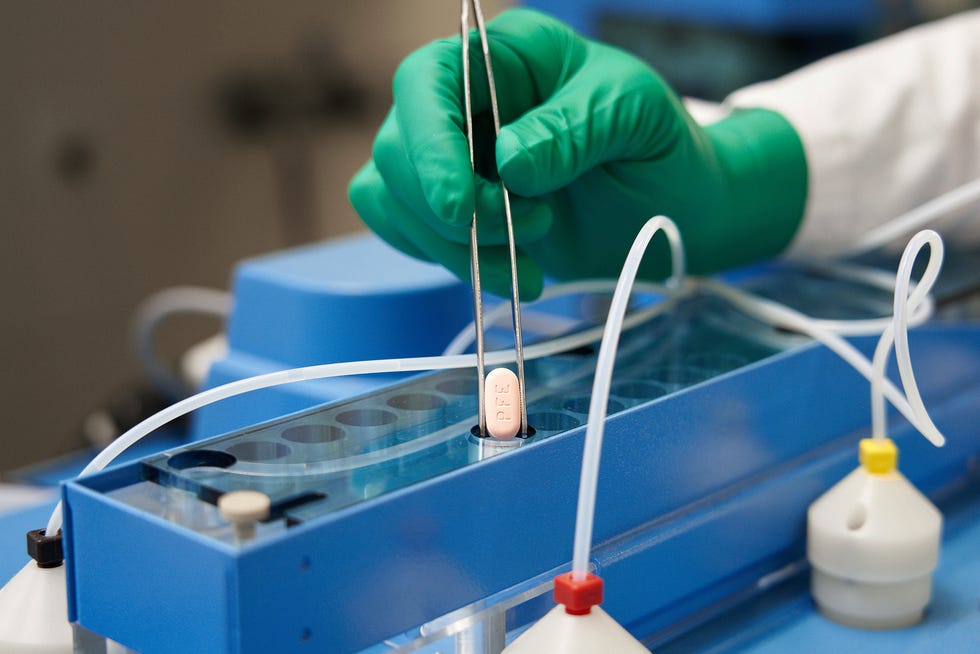
Some doctors are hesitant to provide the antiviral because people may need to stop taking common medications during the five-day treatment course, but it’s essential for people at high risk for serious disease, Hotez said. “Any senior going on Paxlovid is not dying,” he said.
“We can’t stop people getting infected,” Cannon added, “but we absolutely can stop people from being seriously ill. Gosh, why wouldn’t you take it?”
Why it’s better not to get infected
Every COVID-19 infection increases your risk for serious disease and for long COVID, which brings sometimes debilitating symptoms that can linger for a year or more.
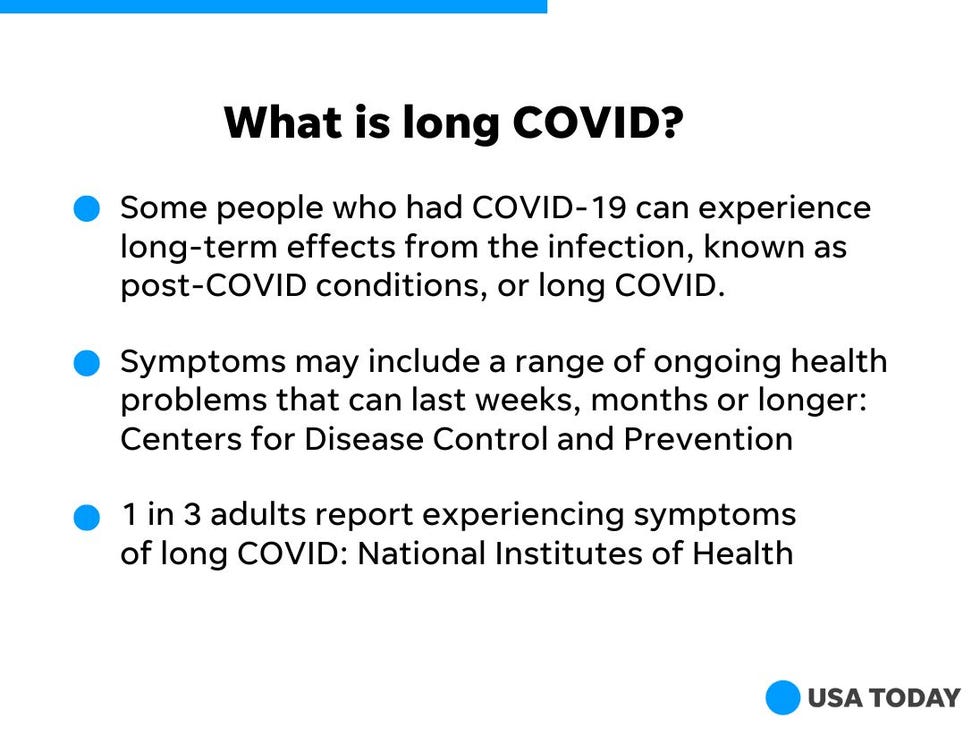
Older adults are more vulnerable, Al-Aly said, “but it doesn’t mean younger people are totally shielded.” Long COVID, too, can strike people at any age from childhood through to the 101-year-old recently treated at his hospital, he said.
Vaccination reduces the risk of long COVID by 15% to 30%, according to a study he recently published. Another study he is working on shows Paxlovid reduces the risk by 26%.
Cannon’s daughter works in a long COVID clinic and regularly sees patients who are in their 20s or 30s, “healthy people who didn’t even have a particularly bad bout of COVID who now have a massively debilitating set of symptoms.”
All six experts interviewed by USA TODAY this week dismissed the idea that there is somehow an upside to getting infected. While an infection might help provide some protection against future infection, vaccination offers better protection without the risk, Al-Aly said.
And getting sick with a virus provides absolutely no benefit, Cannon said.
“I’d be happy if I never got any virus again. And I say this as a professional virologist.”
Could we be nearing the end of COVID?
COVID-19 has been perhaps the most successful virus in all of human history, Cannon said, infecting billions of people across the planet.
While she worries about how it might continue to evolve, she hopes it’s a good sign that for the last year, all the variants have been descendants of omicron.
Before that, the original virus, alpha, beta and delta had been “radically” different from each other.
“The virus is now in this committed lineage,” Cannon said, which might mean it won’t evolve away from the protection against serious disease that nearly everyone now has from vaccinations and previous infections.
Contact Karen Weintraub at kweintraub@usatoday.com.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.